Guideline 11.10 Resuscitation in special circumstances
Summary
Who does this guideline apply to?
This guideline applies to adults who require advanced life support ALS.
Who is the audience for this guideline?
This guideline is for health professionals and those who provide healthcare in environments where equipment and drugs are available.
Guideline
Most sudden cardiac arrests are associated with coronary heart disease, but up to 30% of out-of-hospital events are believed to be of a non-cardiac cause. These conditions account for a large proportion of cardiac arrests in young patients with no co-existing disease. Early recognition and effective treatment of these conditions may prevent cardiac arrest or increase the chance of a successful outcome. Survival in all these conditions still relies on using the ABCDE Airway, Breathing, Circulation, Disability, Exposure approach.
Resuscitation needs to be modified in specific circumstances and may require specialist interventions. If cardiac arrest does occur, high quality cardiopulmonary resuscitation CPR with minimal interruption and treatment of reversible causes are still the most important interventions.
These topics are also covered in the Australian Resuscitation Council & New Zealand Resuscitation Council Advanced Life Support Course Manuals.
Anaphylaxis
The World Allergy Organisation Anaphylaxis Committee defines anaphylaxis as:
A serious systemic hypersensitivity reaction that is usually rapid in onset and may cause death.
Severe anaphylaxis is characterised by potentially life-threatening compromise in airway, breathing, and/or circulation,
and may occur without typical skin features or circulatory shock being present.1
The Australasian Society of Clinical immunology and Allergy ASCIA define anaphylaxis as:
Any acute onset illness with typical skin features urticarial rash or erythema/flushing, and/or angioedema, plus involvement of respiratory and/or cardiovascular and/or persistent severe gastrointestinal symptoms; or any acute onset of hypotension or bronchospasm or upper airway obstruction where anaphylaxis is considered possible, even if typical skin features are not present.
Recent reviews, recommendations, and resources related to anaphylaxis are available from ASCIA Acute Management of Anaphylaxis 2023, https://www.allergy.org.au/hp/papers/acute-management-of-anaphylaxis-guidelines , the Australian and New Zealand College of Anaesthetists (ANZCA) and Australian and New Zealand Anaesthetic Allergy Group ANZAAG perioperative anaphylaxis guidelines at https://www.anzca.edu.au/safety-advocacy/standards-of-practice/perioperative-anaphylaxis-management-guidel, and the Resuscitation Council UK Emergency treatment of anaphylaxis: Guidelines for healthcare providers 2021 at https://www.resus.org.uk/library/additional-guidance/guidance-anaphylaxis.2-4
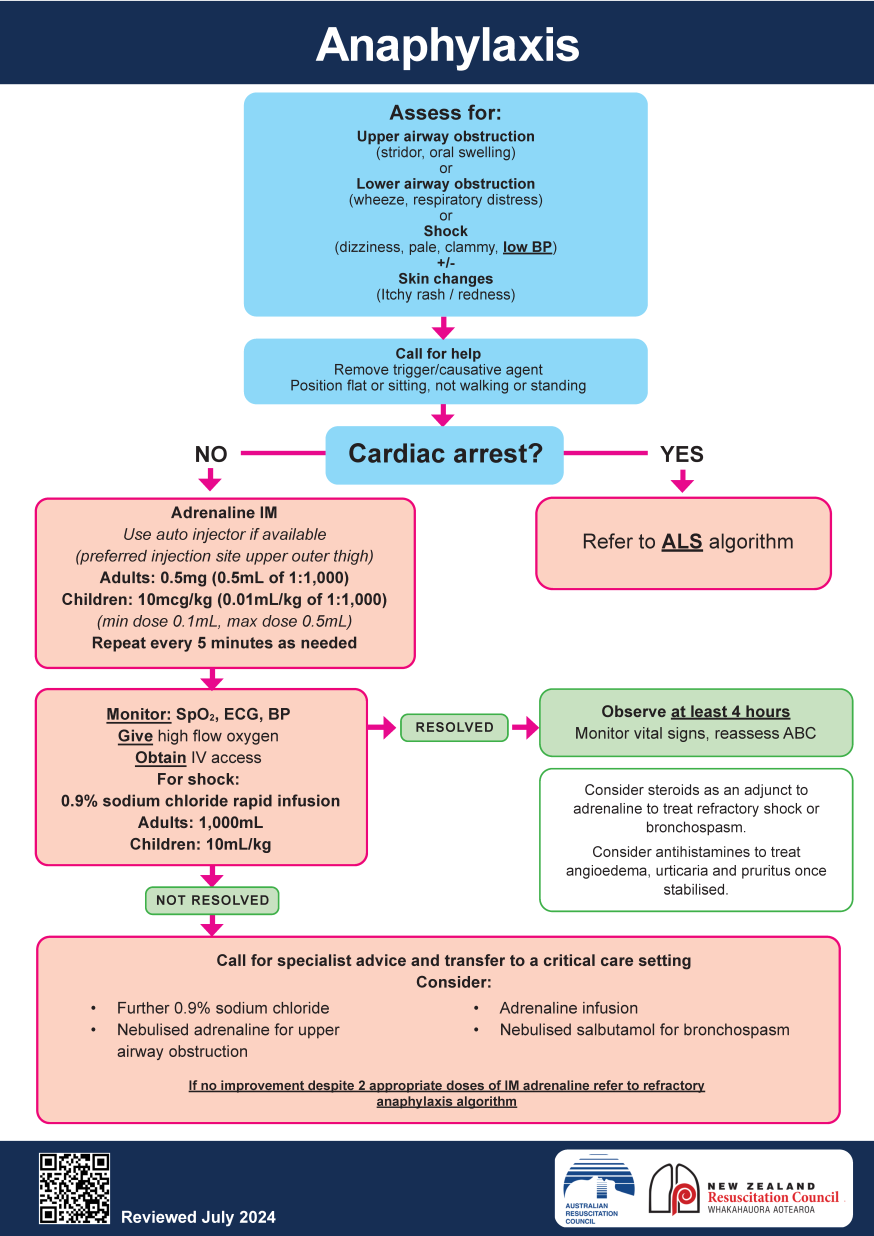
For non-cardiac arrest anaphylaxis situations these resources place increased emphasis on:
- Recognising anaphylaxis based on sudden onset and rapid progression of symptoms e.g. Airway and/or Breathing and/or Circulation problems, skin and/or mucosal changes flushing, urticaria, angioedema.
- Treating life-threatening features, using the Airway, Breathing, Circulation, Disability, Exposure ABCDE approach.
- Adrenaline is the first-line treatment for anaphylaxis. Give intramuscular IM adrenaline early in the anterolateral thigh for Airway/Breathing/Circulation
- Repeat IM adrenaline after 5 minutes if Airway/Breathing/Circulation problems persist.
- Intravenous IV adrenaline must only be used in certain specialist settings, and only by those skilled and experienced in its use.
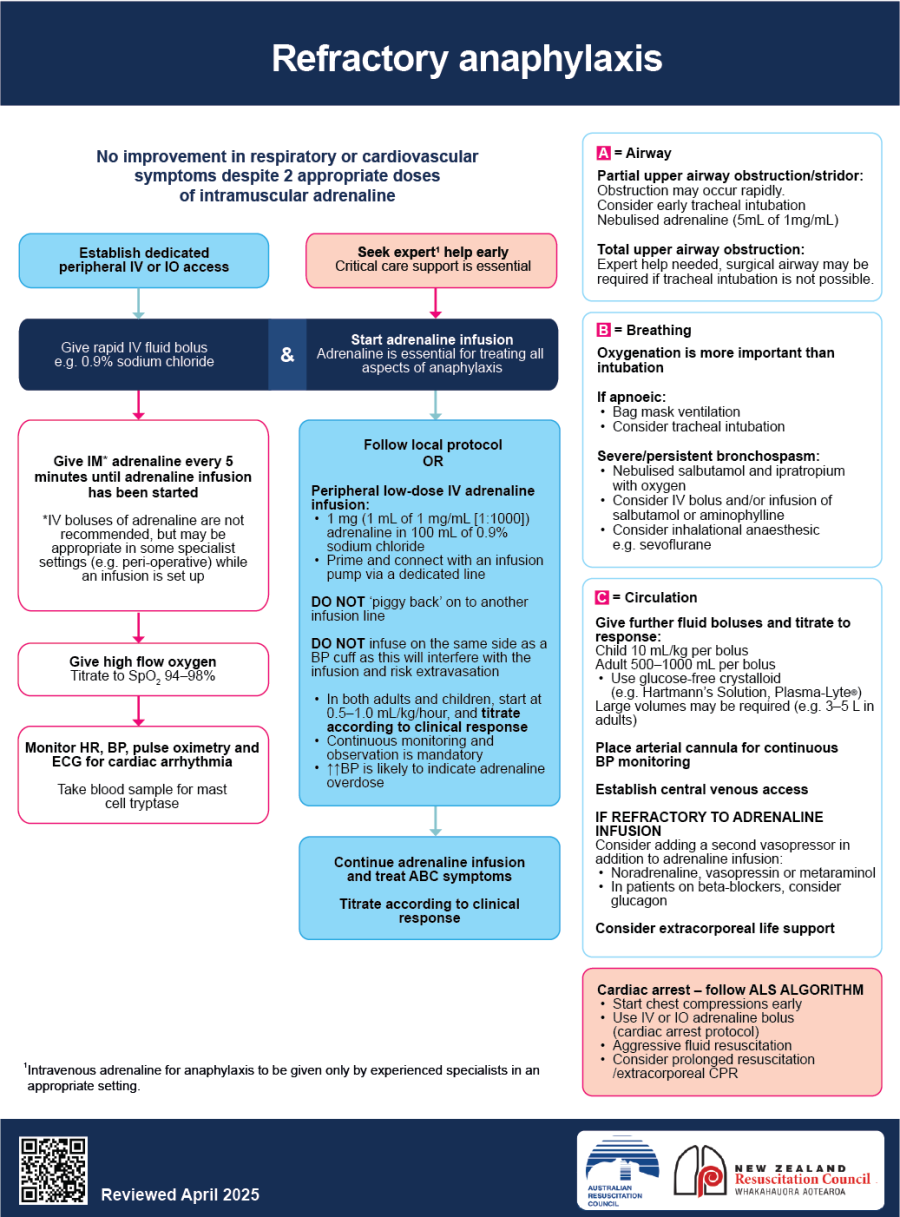
Refractory anaphylaxis
Recognising refractory anaphylaxis is based on no improvement in respiratory and/or cardiovascular symptoms despite 2 doses of IM adrenaline.
Seek expert help early in patients with refractory anaphylaxis.
IV adrenaline infusions form the basis of treatment for refractory anaphylaxis.
IV bolus adrenaline commencing at 10 to 20 micrograms escalating by doubling dose if unresponsive may be considered by those experienced in its use while infusions are prepared e.g. for anaphylaxis associated with anaesthesia, and anaphylaxis management in the Emergency Department or Intensive Care Unit ICU.
Additional vasopressors and inotropes may be considered.
Nebulised adrenaline may be effective in treating upper airway oedema.
Large volumes of IV crystalloid e.g. 0.9% sodium chloride or Hartmann’s Solution may be required.
Airway obstruction may occur rapidly.
Tracheal intubation may be considered early and should involve experts in airway management.
A surgical airway may be required if tracheal intubation is not possible.
Antihistamines and corticosteroids are not recommended routinely. Corticosteroids may be considered as an adjunct to adrenaline to treat refractory shock or bronchospasm. Antihistamines can be useful to treat angioedema, urticaria and pruritus once patients have been stabilised.
Extracorporeal cardiopulmonary resuscitation ECPR may be considered for refractory anaphylaxis.
Recommendations
Anaphylaxis treatment in cardiac arrest
Australian and New Zealand Committee on Resuscitation ANZCOR suggests that if anaphylaxis results in cardiorespiratory arrest, the advanced life support ALS protocol should be followed, as well as giving large volumes of intravenous fluids. Additional vasopressors (noradrenaline, vasopressin, metaraminol) may be considered. Prolonged resuscitation may be necessary and ECPR may be considered Good Practice Statement.
Anaphylaxis treatment in the non-cardiac arrest situation
ANZCOR treatment of anaphylaxis algorithm
ANZCOR Treatment of Refractory Anaphylaxis
(modified with permission from RCUK)
View and Download a copy of the Refractory Anaphylaxis flowchart: Refractory Anaphylaxis Flowchart
ANZCA Perioperative Anaphylaxis Management Guidelines are available at:
(https://www.anzca.edu.au/safety-advocacy/standards-of-practice/perioperative-anaphylaxis-management-guidel)
Asthma
Cardiac arrest in the asthmatic is often a terminal event after a period of hypoxaemia; occasionally, it may be sudden.
Cardiac arrest in asthmatics has been linked to:
- severe bronchospasm and mucous plugging leading to asphyxia
- cardiac arrhythmias due to hypoxia, or arrhythmias due to stimulant drugs (e.g. beta-adrenergic agonists, aminophylline) or electrolyte abnormalities
- dynamic hyperinflation, i.e. auto-positive end-expiratory pressure (auto-PEEP), can occur in mechanically ventilated asthmatics. Auto-PEEP is caused by air trapping and ‘breath stacking’ (air entering the lungs and being unable to escape). Gradual build-up of pressure occurs and reduces venous return and blood pressure
- tension pneumothorax (occasionally bilateral).
There are no randomised controlled trials that specifically evaluate or compare adjuvant treatment with standard treatment for cardiac arrest in asthmatics. Most of the literature comprises case reports and case series.5
Recommendations
Follow standard basic life support (BLS) and ALS protocols. Ventilation will be difficult because of increased airway resistance; try to avoid gastric inflation [Good Practice Statement].
Intubate the trachea early. There is a significant risk of gastric inflation and hypoventilation of the lungs when attempting to ventilate a severe asthmatic without a tracheal tube (Good Practice Statement).
Use a slow respiratory rate (<10 breaths per min) and low tidal volumes which may be less likely to cause dynamic hyperinflation of the lungs (gas trapping) (Good Practice Statement).
If dynamic hyperinflation of the lungs is suspected during CPR, compression of the chest wall and/or a period of apnoea (disconnection of tracheal tube) may relieve gas-trapping (Good Practice Statement).
Dynamic hyperinflation increases transthoracic impedance, but this is not thought to reduce the efficacy of modern biphasic defibrillators. As with standard ALS, consider increasing manual defibrillator energy if the first shock is unsuccessful (Good Practice Statement).
Look for reversible causes using the 4 Hs and 4 Ts approach (Good Practice Statement).
Consider tension pneumothorax (including bilateral) (Good Practice Statement).
Consider Extracorporeal cardiopulmonary resuscitation (ECPR) (Good Practice Statement).
Avalanches
Avalanches occur in areas that are difficult to access by rescuers in a timely manner, and frequently involve multiple victims. The decision to initiate full resuscitative measures should be determined by the number of victims and the resources available and should be informed by the likelihood of survival.
Avalanche victims are not likely to survive when they are:
- buried > 35 minutes and in cardiac arrest with an obstructed airway on extrication
- buried initially and in cardiac arrest with an obstructed airway on extrication, and an initial core temperature of <32 degrees
- buried initially and in cardiac arrest on extrication with an initial serum potassium of >12 mmol.
Recommendations
Full resuscitative measures, including extracorporeal rewarming, when available, are indicated for all avalanche victims who do not show evidence of a non-survivable injury (Good Practice Statement).5,6
Cardiac Surgery
After major cardiac surgery, cardiac arrest is relatively common in the immediate post-operative phase. Cardiac arrest is usually preceded by physiological deterioration, although it may occur suddenly in stable patients. Continuous monitoring in an ICU enables immediate intervention at the time of arrest. Survival to hospital discharge of patients having a cardiac arrest during the first 24 hours after cardiac surgery is higher than other patient groups.
There are usually specific causes of cardiac arrest and these are all potentially reversible. The main causes of cardiac arrest in the initial post-operative period include:
- cardiac tamponade
- haemorrhage causing hypovolaemic shock
- myocardial ischaemia
- tension pneumothorax
- pacing failure.
ANZCOR endorses the Australasian Australian and New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) and Australian and New Zealand Intensive Care Society (ANZICS) guidelines on cardiothoracic advanced life support (CALS-ANZ).7
These guidelines highlight key differences to standard ALS:
- Prolonged periods of external chest compressions can cause significant damage to thoracic structures in the early postoperative phase and may be ineffective in an arrest due to tamponade or hypovolemia.
- Emergency re-sternotomy is an integral part of the CALS protocol and should be completed by a trained team within 5 minutes from the onset of the cardiac arrest.
- Internal cardiac compression is generally more effective than external cardiac compression.
- Most reversible causes of cardiac arrests are addressed by an emergency re-sternotomy.
ANZCOR recommends use of the CALS-ANZ algorithm to assess and manage cardiac surgical patient in cardiac arrest. Based on methodology the recommendations can be considered Good Practice Statements.
The algorithm recommends three treatment pathways:
- If the patient is in pulseless ventricular tachycardia (VT) or ventricular fibrillation (VF) cardiac arrest, adhesive defibrillator pads are attached and up to three stacked shocks are delivered.
- If the patient is in asystole or severe bradycardia with epicardial pacing wires in place, the patient is paced in DOO mode.
- If the patient is in pulseless electrical activity arrest and is paced at the time of the arrest, the pacemaker is briefly paused to exclude underlying ventricular fibrillation (which would require defibrillation).
During this initial phase of assessment and management, external chest compressions may be withheld for up to 60 seconds.
If these initial measures fail to establish ROSC re-sternotomy should be performed to address reversible factors.
Chest compressions should not be withheld while preparing for emergency re-sternotomy.
Transthoracic or trans-oesophageal echocardiography may be useful when readily available to help elucidate the cause of the cardiac arrest (including haemoperitoneum, haemothorax, tension pneumothorax and cardiac tamponade).
Mechanical circulatory support may also be considered in the setting of cardiac arrest following cardiac surgery.
CALS-ANZ Cardiothoracic Advanced Life Support
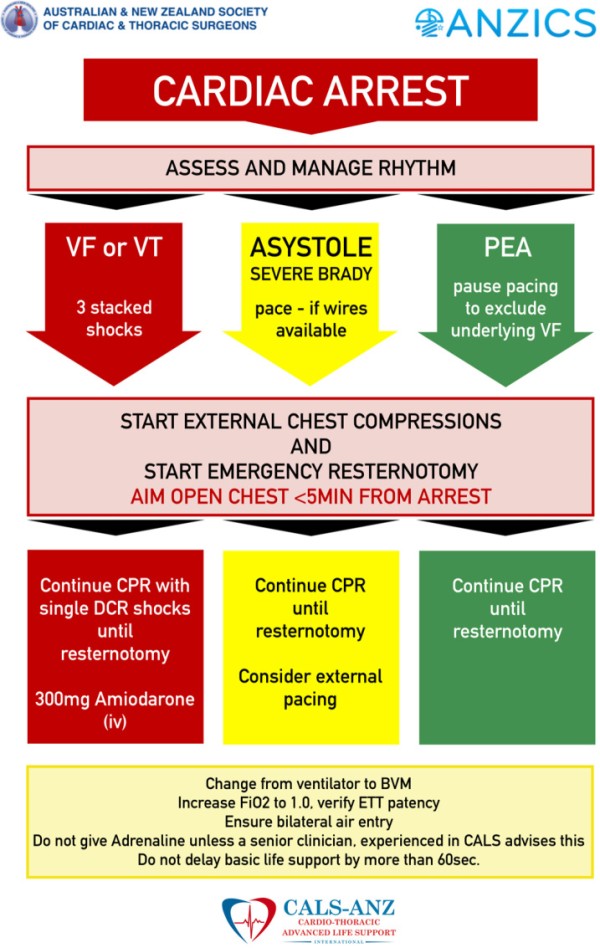
Reproduced with permission from Critical Care and Resuscitation7
Drowning
Initial resuscitation once retrieved from water
The drowning person rescued from the water within a few minutes of submersion is likely to exhibit abnormal (agonal) breathing. Do not confuse this with normal breathing.
Give 5 initial ventilations, supplemented with oxygen if available.
If the person has not responded to initial ventilations, place them on a firm surface before starting chest compressions. Provide CPR in a ratio of 30 compressions to 2 ventilations. Most drowning people will have sustained cardiac arrest secondary to hypoxia. In these patients, compression-only CPR is likely to be ineffective and should be avoided.
Massive amounts of foam caused by mixing air with water and surfactant can sometimes come out of the mouth of people. If this occurs, continue rescue breaths/ventilation until an ALS provider arrives and is able to intubate the person’s trachea.
Regurgitation of stomach contents and swallowed water is common. If this prevents ventilation, turn the person on their side and remove the regurgitated material using directed suction if possible.
(Good Practice Statements)
Modifications to advanced life support after drowning
Airway and breathing
Give high-flow oxygen (10 to 15 L /min), ideally through a non-rebreather mask with reservoir to the spontaneously breathing person.
For people who fail to respond to initial basic airway measures, who have a reduced level of consciousness or are in cardiac arrest, consider early tracheal intubation and controlled ventilation by skilled personnel. Reduced pulmonary compliance requiring high inflation pressures may limit the use of a supraglottic airway device.
In non-fatal drowning when the person who has not arrested or has achieved ROSC, titrate the inspired oxygen concentration to achieve an SpO2 of 94 to 98%. Confirm adequate oxygenation and ventilation with arterial blood gases once available. Set positive end expiratory pressure (PEEP) to at least 5 to 10 cm H2O. However, PEEP values of 15 to 20 cm H2O may be required if the patient is severely hypoxaemic. Decompress the stomach with a gastric tube.
(Good Practice Statements)
Circulation and defibrillation
Palpation of the pulse as the sole indicator of the presence or absence of cardiac output is not always reliable, particularly in the wet and cold drowning patient. As soon as possible, check the ECG and end-tidal CO2 (EtCO2) and consider echocardiography to confirm the presence or not of a cardiac output.
If the person is in cardiac arrest, follow standard ALS protocols. If the person is hypothermic, modify the approach in accordance with the guidance for treatment of hypothermia (see below).
Assess the rhythm and attempt defibrillation if indicated according to standard guidelines. Dry the person’s chest before applying defibrillator pads.
After prolonged immersion, most people will have become hypovolaemic as the hydrostatic pressure of water on the body is removed. Give rapid IV fluid to correct hypovolaemia. This should commence out-of-hospital, if transfer time is prolonged.
Consider ECPR in accordance with local protocols if initial resuscitation efforts are unsuccessful.
(Good Practice Statements)
Discontinuing resuscitation efforts
The decision to discontinue resuscitation efforts on a person of drowning is difficult. No single factor accurately predicts good or poor survival.
Continue resuscitation unless there is clear evidence that such attempts are futile (e.g. massive traumatic injuries, rigor mortis, putrefaction etc.), or timely evacuation to a medical facility is not possible.
Neurologically favourable outcomes have been reported in several people submerged for longer than 25 min, however these rare case reports almost invariably occur in children submerged in ice-cold water, when immersion hypothermia has preceded hypoxia or in submersion of car occupants. Outcomes are extremely poor if ALS takes longer than 30 min to achieve ROSC even if hypothermia is present.
(Good Practice Statements)
Electrolyte disorders
(Refer to ANZCOR Guideline 11.5 Medications in Adult Cardiac Arrest).
Electrolyte abnormalities can cause cardiac arrhythmias or cardiorespiratory arrest. Life-threatening arrhythmias are most commonly associated with potassium disorders, particularly hyperkalaemia, and less commonly with disorders of serum calcium and magnesium.
Treat life-threatening electrolyte abnormalities before cardiac arrest occurs. Remove precipitating factors (e.g. drugs, diet) and monitor electrolyte concentrations to prevent recurrence of the abnormality. Monitor renal function in patients at risk of electrolyte disorders (e.g. patients with acute and chronic kidney disease, heart failure) and avoid combinations of drugs that may exacerbate electrolyte disorders. Review renal replacement therapy (e.g. haemodialysis) regularly to avoid inappropriate electrolyte shifts during treatment.
(Good Practice Statements)
Modifications to CPR associated with hyperkalaemia
Confirm hyperkalaemia using a blood gas analyser if available.
Protect the heart: give 10 mL calcium chloride 10% IV (or 30 ml Calcium Gluconate) by rapid bolus injection. Consider repeating dose if cardiac arrest is prolonged or refractory.
To shift potassium into cells: give glucose/insulin: 10 units short-acting insulin and 25 g glucose (50mls of 50% glucose) IVI. Monitor blood glucose levels.
If severe acidosis or renal failure give sodium bicarbonate: 50 mmol (50 mL of 8.4% solution) IV by rapid injection. Avoid mixing with calcium chloride as may cause a precipitate.
To remove potassium from body: consider dialysis for hyperkalaemic cardiac arrest resistant to medical treatment. Several dialysis modalities have been used safely and effectively in cardiac arrest, but this may only be available in specialist centres.
Consider the use of a mechanical chest compression device if prolonged CPR is needed.
(Good Practice Statements)
Hypothermia
Hypothermia exists when the body core temperature is below 35˚C and is classified arbitrarily as mild (32 to 35°C), moderate (28 to 32°C), or severe (< 28°C).
Core temperature is best assessed with a low reading thermometer; tympanic (thermocouple device) in spontaneously breathing, oesophageal (distal) in patients with a tracheal tube or a supraglottic device. Commonly used tympanic thermometers based on infrared technique do not seal the ear canal and are not designed for low core temperature readings.
Check for the presence of vital signs for up to one minute. Palpating a central artery, assessing cardiac rhythm, capnography, and echocardiography may assist in identifying cardiac output.
Prehospital insulation, triage, fast transfer to a hospital and rewarming are key interventions.
Hypothermic patients with high risk for imminent cardiac arrest (i.e. core temperature < 30°C, ventricular arrhythmia, systolic blood pressure < 90 mmHg) and those in cardiac arrest should directly transferred to an extracorporeal life support (ECLS) centre for rewarming if available.
Hypothermic cardiac arrest patients should receive continuous CPR during transfer, with compression and ventilation rates the same as for normothermic patients. Intermittent CPR during rescue can be of benefit if continuous CPR cannot be delivered.
Consider the use of a mechanical chest compression device if prolonged CPR is needed.
The hypothermic heart may be unresponsive to cardioactive drugs, attempted electrical pacing and defibrillation. If VF persists after three shocks, delay further attempts until the core temperature is > 30°C.
Withhold adrenaline if the core temperature is < 30°C. Increase administration intervals for adrenaline to 6 to 10 minutes if the core temperature is 30 to 34°C.
Do not delay tracheal intubation when it is indicated.
In hypothermic cardiac arrest, rewarming should be performed with ECLS (extracorporeal membrane oxygenation (ECMO) is preferred over cardiopulmonary bypass). Non-ECLS rewarming should be initiated in a peripheral hospital if an ECLS centre cannot be reached.
Rewarming general principles:
- Remove from the cold environment, prevent of further heat loss and rapid transfer to hospital.
- Remove wet clothes, while minimising excessive movement of the person.
- Rewarming may be passive, active external, or active internal.
- Passive rewarming is appropriate as patients are still able to shiver, and achieved by full body insulation with wool blankets, aluminium foil, cap, and a warm environment.
- Active external rewarming involves chemical heat packs and forced warm air. Minimally invasive methods include warm intravenous fluids and warm humidified gases. Non-ECLS centre rewarming may combine external and internal rewarming techniques (e.g. forced warm air, warm infusions, peritoneal lavage).
(Good Practice Statements)
Percutaneous Coronary Interventions
There is evidence of underlying ischemic heart disease in the majority of patients who have cardiac arrests. Recommendations for the use of angiography and percutaneous coronary intervention (PCI) in the setting of cardiac arrest are included in ANZCOR Guideline 11.7 Post-Resuscitation Therapy in Adult Advanced Life Support. Refer also to ANZCOR Guideline 14.3 Acute Coronary Syndromes: Reperfusion Strategy.
Recommendations
Mechanical CPR during PCI
ANZCOR suggests that automated mechanical chest compression devices are a reasonable alternative to high-quality manual chest compressions in situations where sustained high-quality manual chest compressions are impractical or compromise provider safety (CoSTR 2015, weak recommendation, low quality evidence).
Cough CPR
Cough CPR may be considered only for patients maintaining consciousness during the initial seconds to minutes of VF or pulseless VT cardiac arrest in a witnessed, monitored, hospital setting (such as a cardiac catheterisation laboratory) (Good Practice Statement).
Pericardial tamponade
The management of pericardial tamponade after cardiac surgery should follow the CALS-ANZ recommendations outlined above.
In the non-cardiac surgery population case series indicate that echocardiography guided pericardiocentesis is a safe and effective method of relieving tamponade, especially when used in conjunction with a pericardial drain, and it may obviate the need for subsequent treatment in the operating room.5
Recommendations
Pericardial tamponade in nontraumatic arrests
Pericardiocentesis guided by ultrasound/echocardiography may be considered for treatment of cardiac arrest associated with suspected cardiac tamponade while non-image guided pericardiocentesis is an acceptable alternative only if echocardiography is not available [Good Practice Statement].
Placement of a pericardial drain may be beneficial and may obviate the need for subsequent operating room treatment [Good Practice Statement].
Emergency room thoracotomy and pericardiotomy can be considered for use in the treatment of non-traumatic cardiac arrest when pericardiocentesis is unsuccessful in relieving cardiac tamponade (Good Practice Statement).
Fluid resuscitation should be continued as indicated while awaiting definitive management (Good Practice Statement).
Pericardial tamponade in traumatic cardiac arrests
(Refer to ANZCOR Guideline 11.10.1 Management of Cardiac Arrest due to Trauma).
The optimal management of pericardial tamponade in traumatic cardiac arrest is definitive surgical drainage and treatment of the underlying cause (Good Practice Statement).
Emergency room thoracotomy and pericardiotomy should be considered as an acceptable alternative to operating room thoracotomy and pericardiotomy for treatment of traumatic cardiac arrest associated with cardiac tamponade (Good Practice Statement).
If neither of the above are possible, pericardiocentesis (ideally with ultrasound guidance) should be attempted (Good Practice Statement).
Fluid resuscitation should be continued as indicated while awaiting definitive management (Good Practice Statement).
Pregnancy
This topic was reviewed in 2015, 2020, and 2024 CoSTR processes.8,9,10
Cardiac arrest in pregnancy is most commonly caused by:
- Cardiac disease
- Pulmonary thrombo-embolism
- Haemorrhage
- Sepsis
- Hypertensive disorders of pregnancy
- Poisoning and self-harm
- Amniotic fluid embolism
- Pregnant women can also have the same causes of cardiac arrest as females of the same age group (e.g. anaphylaxis, drug overdose, trauma).
The physiological changes associated with pregnancy (increased cardiac output, blood volume, minute ventilation, oxygen consumption and reduced lung volumes) complicate basic management of the airway, breathing, circulation (ABCs). Hypoxia occurs quickly, intubation is more difficult and gastric reflux is more likely. The gravid uterus (after 20 weeks) causes compression of the abdominal organs and iliac and abdominal vessels when the mother is in the supine position. This results in reduced cardiac output and hypotension. There are no randomised controlled trials evaluating the effect of specialised obstetric resuscitation versus standard care in post-arrest pregnant women.
Resuscitation guidelines for pregnancy are based largely on case series, extrapolation from non-pregnant arrests, manikin studies and expert opinion based on the physiology of pregnancy and changes that occur in normal labour.
Treatment may be guided by understanding the physiology of pregnancy, the importance of releasing aortocaval compression, the increased risk for hypovolemia, the compression advantage through positioning and the value of caesarean section early in maternal cardiac arrest.5,11
Recommendations
In cardiac arrest, all the principles of basic and advanced life support apply. Although there is concern for the viability of the unborn child, effective resuscitation of the mother is the best way to optimise foetal outcome (Good Practice Statement).
Summon expert help immediately.
ANZCOR suggests, if over 20 weeks or the uterus is palpable above the umbilicus, manual displacement of the uterus to the left to relieve aortocaval compression. If left lateral tilt is added, the angle needs to allow high quality chest compressions and permit surgical delivery of the foetus if this is to be done (between 15 and 30 degrees has been suggested as feasible) (Good Practice Statement).
ANZCOR suggest delivery of the fetus by perimortem cesarean delivery for women in cardiac arrest in the second half of pregnancy (CoSTR 2020, weak recommendation, very low-quality evidence).
There is insufficient evidence to define a specific time interval by which delivery should begin.
High-quality usual resuscitation care and therapeutic interventions that target the most likely cause(s) of cardiac arrest remain important in this population (Good Practice Statement).
ECPR may be considered as a rescue therapy for selected cardiac arrest patients during pregnancy or in the postpartum period when conventional CPR fails and in settings in which it can be implemented [Good Practice Statement].
Institution readiness and resuscitation education are required to accommodate the unique physiologic challenges of cardiac arrest during pregnancy (Good Practice Statement).
Pulmonary embolus
Pulmonary embolism (PE) is a potentially reversible cause of cardiac arrest. This topic was reviewed in 2015 and 2020. No RCTs were identified, and no meta-analysis was undertaken given the limited evidence. It is considered that 2% to 7% of patients with out-of-hospital cardiac arrests (OHCA) have a PE and this figure is probably higher for patients with in-hospital cardiac arrests (IHCA). ECPR techniques are also being used in patients with cardiac arrest from suspected PE. This role of ECPR in patients with PE is unclear but may potentially facilitate the use of fibrinolysis or mechanical or surgical embolectomy. There is an increased risk of bleeding from fibrinolysis if it is administered to patients without PE. Patients are more likely to die from the cardiac arrest than from the treatment.
Recommendations
ANZCOR suggests administering fibrinolytic drugs for cardiac arrest when PE is the suspected cause of cardiac arrest (CoSTR 2020, weak recommendation, very low-certainty evidence).
ANZCOR suggests the use of fibrinolytic drugs or surgical embolectomy or percutaneous mechanical thrombectomy for cardiac arrest when PE is the known cause of cardiac arrest (CoSTR 2020, weak recommendation, very low certainty evidence).
If a fibrinolytic drug is given in these circumstances, consider performing CPR for 60 to 90 min before termination of resuscitation attempts (Good Practice Statement).
Refer also to ANZCOR Guideline 11.5 Medications in Adult Cardiac Arrest.
Tension pneumothorax
Tension pneumothorax may be the cause of cardiac arrest or develop during a cardiac arrest as positive pressure ventilation may convert a non-tension pneumothorax into a tension pneumothorax.
Diagnosis is based on clinical assessment, ultrasound or X-ray.
In cardiac arrest patients with a suspected tension pneumothorax, the chest cavity should be immediately decompressed:
Needle-cannula decompression either in the 2nd intercostal space (just above the 3rd rib) mid-clavicular line, or the 4th/5th intercostal space in the mid-axillary line, should be followed by chest drain insertion.
An open thoracostomy technique is an alternate initial approach for those trained, and then followed by chest drain insertion.
(Good Practice Statements)
Three stacked shocks
There are some situations where the patient develops a shockable rhythm in a witnessed and monitored setting and the defibrillator is immediately available (e.g. first shock able to be delivered within 20 seconds). This may occur in the pre-hospital setting, emergency department, critical care and coronary care unit, cardiac catheter laboratory or the operating room. In these settings it may be appropriate to use a 3 stacked-shock technique (i.e. without commencing chest compressions between shocks), especially where there may be a relative contraindication to external cardiac compressions (e.g. after cardiac surgery).
The “3 stacked-shock sequence” (delivery of up to three shocks if needed) can be optimised by immediate rhythm analysis and charging of the defibrillator. This protocol may be of benefit in scenarios where the first shock is able to be delivered within 20 seconds, the time required for rhythm recognition and for recharging the defibrillator is short (i.e. <10 seconds). The trade-off is interruptions in external cardiac compressions, so the patients need to be in a well-oxygenated, well-perfused state immediately before the arrest.
Recommendations
A sequence of up to 3 stacked shocks should be considered in cardiac arrest patients who develop a shockable rhythm where the setting is:
- a witnessed and monitored arrest, and
- the defibrillator is immediately available (e.g. first shock able to be delivered within 20 seconds), and
- the time required for rhythm recognition and for recharging the defibrillator is short (i.e. <10 seconds).
(Good Practice Statements)
If the patient does not have return of spontaneous circulation within 10 seconds of the delivery of the third shock, compressions should be started immediately. If after any shock the non-cardiac surgical patient develops a non-shockable rhythm, but does not have ROSC within 10 seconds, compressions should be started immediately. Follow the CALS algorithm above for cardiac surgical patients (Good Practice Statement).
Toxins
Poisoning is a leading cause of death in those younger than 40 years. It is also a common cause of non-traumatic coma in this age group. Self-poisoning with therapeutic or recreational drugs, and therapeutic drug toxicity are leading causes of hospital admission.
14.1 Preventing cardiac arrest
Assess and treat the patient using the ABCDE approach. Manage severe poisoning in a critical care setting. Airway obstruction, aspiration and respiratory arrest due to decreased consciousness is a common cause of death after self-poisoning. Early tracheal intubation can decrease these risks. Drug-induced hypotension usually responds to IV fluids, but vasopressor support may be required. Measure electrolytes (particularly potassium), blood glucose and arterial blood gases. Retain samples of blood and urine for analysis.
14.2 Modifications to resuscitation
- Ensure personal safety and wear personal protective equipment (PPE).
- Avoid mouth-to-mouth rescue breaths in the presence of toxic chemicals e.g. organophosphates and corrosives.
- Treat life-threatening tachyarrhythmias with cardioversion.
- Try to identify the toxin(s) from history and examination (odours, needle marks, pupil size, and signs of corrosion in the mouth).
- Monitor temperature because hypo- or hyperthermia can occur after drug overdose.
- Provide standard basic and advanced life support if cardiac arrest occurs.
- Be prepared to continue resuscitation for a prolonged period, particularly in young patients, as the poison may be metabolised or excreted during extended resuscitation measures. Consider ECPR if the toxicity is potentially reversible.
(Good Practice Statements)
Poisons information centres in Australia offer advice on risk assessment and management of suspected poisonings, including injuries by venomous animals. They coordinate to provide services across Australia 24 hours a day—telephone 13 11 26.
In New Zealand there is a single National Poisons Centre based in Dunedin, which provides telephone advice 24hours a day – telephone 0800 764 766
14.3 Specific treatments
The emphasis is on intensive supportive therapy using the ABCDE approach, with correction
of hypoxia, hypotension, acid/base, and electrolyte disorders.
Therapies include decontamination, limiting absorption of ingested poisons, enhancing elimination, and, when available, the use of specific antidotes.
- To prevent ongoing skin exposure to toxins, remove clothes.
- Routine use of gastric lavage is not recommended.
- Consider giving a single dose of activated charcoal to patients who have ingested a potentially toxic amount of a poison known to be adsorbed by activated charcoal, up to one hour previously. Give only to patients with an intact or protected airway. Multiple doses may be beneficial in life-threatening poisoning with carbamazepine, dapsone, phenobarbital, quinine and theophylline.
- Consider whole-bowel irrigation using a polyethylene glycol solution in potentially toxic ingestion of sustained release or enteric-coated drugs, oral iron poisoning, and the removal of ingested packets of illicit drugs.
- Laxatives and emetics are not recommended.
- Urinary alkalinisation (urine pH > 7.5) using IV sodium bicarbonate can be considered in salicylate poisoning in patients who do not need haemodialysis.
- Haemodialysis removes drugs or metabolites with low molecular weight, low protein binding, small volumes of distribution and high-water solubility.
- Specific antidotes should be employed in the appropriate clinical context to prevent deterioration to cardiac arrest. During cardiac arrest there is little evidence to support the use of these specific antidotes. ECPR may be considered.
(Good Practice Statements)
14.4 Specific antidotes
Naloxone
Opioid poisoning causes respiratory depression, pinpoint pupils and coma followed by respiratory arrest. Naloxone rapidly reverses these effects and can be administered IV, intraosseous (IO), IM, subcutaneous (SC), and intranasal (IN) routes. The initial doses of naloxone are 400 mcg IV, 800 mcg IM, 800 mcg SC or 2 mg IN. Large opioid overdoses may require titration to a total naloxone dose of 10 mg. The duration of action of naloxone is 45 to 70 minutes, but respiratory depression may persist for 4 to 5 hours after opioid overdose. Thus, the clinical effects of naloxone may not last as long as those of a significant opioid overdose. Give increments of naloxone until the patient is breathing adequately and has protective airway reflexes. Consider the need for an ongoing infusion of naloxone if the respiratory rate is not maintained and long-acting opioid preparations have been ingested. Acute withdrawal from opioids produces a state of sympathetic activation and can cause complications such as pulmonary oedema, ventricular arrhythmia, and severe agitation. Use naloxone reversal of opioid intoxication with caution in patients suspected of opioid dependence. Cardiac arrest is usually secondary to a respiratory arrest and associated with severe brain hypoxia and the prognosis is poor. Once cardiac arrest has occurred, follow standard resuscitation guidelines.
There are no RCTs evaluating conventional versus alternative treatments for cardiac arrest caused by opioids. Evidence is limited to studies of mild, moderate, and severe cardiovascular toxicity. Evidence from studies assessing other endpoints (efficacy of naloxone), as well as animal studies, support the use of assisted ventilation before giving naloxone in opioid-poisoned patients with severe cardiopulmonary toxicity.
Recommendations
Respiratory Arrest
ANZCOR recommends the use of naloxone by IV, IM, SC, IO, or IN routes in respiratory arrest associated with opioid toxicity (CoSTR 2015 strong recommendation, very low quality of evidence).8 The dose of naloxone required will depend on the route of administration.
Cardiac Arrest
Lack of comparative data means there is insufficient clinical evidence to make evidence-based treatment recommendations regarding the use of naloxone in cardiac arrest associated with opiate toxicity. If cardiac arrest occurs in the setting of toxicity due to opioids, we suggest following standard resuscitation guidelines (Good Practice Statement).
Flumazenil
Benzodiazepine overdose causes loss of consciousness, respiratory depression and hypotension. Flumazenil, a competitive antagonist of benzodiazepines can be used to reverse sedation caused by benzodiazepines when there is no history or risk of seizures. Reversal of benzodiazepine intoxication with flumazenil can cause significant toxicity (seizure, arrhythmia, hypotension, and withdrawal syndrome) in patients with benzodiazepine dependence or co-ingestion of proconvulsant medications. Do not use flumazenil routinely in the comatose patient. There are no specific modifications required for cardiac arrest caused by benzodiazepines.
Recommendations
Flumazenil may be used with caution to reverse the effects of benzodiazepines (Good Practice Statement).
There are no specific modifications required for cardiac arrest caused by benzodiazepines. Administration of flumazenil during cardiac arrest is not recommended (Good Practice Statement).
Antidotes for drug induced severe bradycardia
Severe bradycardia from poisoning or drug overdose may be refractory to standard ALS protocols because of prolonged receptor binding or direct cellular toxicity. Atropine can be life-saving in organophosphate, carbamate or nerve agent poisoning. Give atropine for bradycardia caused by acetylcholinesterase-inhibitors. Large (2 to 4 mg IV) and repeated doses may be required to achieve a clinical effect. Isoprenaline may be useful at high doses in refractory bradycardia induced by beta-receptor blockade. Heart block and ventricular arrhythmias associated with digoxin or digitalis glycoside poisoning may be treated effectively with digoxin-specific antibody fragments. Vasopressors, inotropes, calcium, glucagon, phosphodiesterase inhibitors and high-dose insulin-glucose-potassium infusions may all be useful in beta-blocker and calcium channel blocker overdose. Transcutaneous and transvenous pacing may be effective for severe bradycardia caused by poisoning and overdose.
(Good Practice Statements)
Hyperbaric oxygen therapy
Patients who develop cardiac arrest caused by carbon monoxide rarely survive to hospital discharge, even if return of spontaneous circulation is achieved. Hyperbaric oxygen therapy may be considered in these patients as it may reduce the risk of developing persistent or delayed neurological injury. The risks inherent in transporting critically ill post-arrest patients to a hyperbaric facility may be significant, and must be weighed against the possibility of benefit on a case-by-case basis.
Recommendations
Following cardiac arrest from carbon monoxide poisoning, hyperbaric oxygen therapy may be considered after return of spontaneous circulation (ROSC) as it may reduce the risk of developing persistent or delayed neurological injury (Good Practice Statement).
Patients who develop myocardial injury caused by carbon monoxide have an increased risk of cardiac and all-cause mortality lasting at least seven years after the event; it is reasonable to recommend cardiology follow-up for these patients (Good Practice Statement).
Antidotes to stimulants
Stimulants include cocaine, and amphetamine (and similar drugs). Sympathetic overstimulation may cause agitation, symptomatic tachycardia, hypertensive crisis, hyperthermia, myocardial ischaemia and infarction. In the non-cardiac arrest situation small doses of intravenous benzodiazepines (midazolam, diazepam, lorazepam) are effective first-line drugs. Glyceryl trinitrate and phentolamine can reverse cocaine-induced coronary vasoconstriction. Use nitrates only as second-line therapy for myocardial ischaemia. The evidence for or against the use of beta-blocker drugs, including those beta-blockers with alpha blocking properties (carvedilol and labetalol) is limited. The optimal choice of anti-arrhythmic drug for the treatment tachyarrhythmias is not known. Seek expert advice if chest pain does not settle, recurs or there is evidence suggesting an acute coronary syndrome.
Recommendations
If cardiac arrest occurs in the setting of toxicity due to cocaine/amphetamines, follow standard resuscitation guidelines (Good Practice Statement).
Antidotes to cyanide poisoning
Case series of the use of several antidotes (hydroxocobalamin, sodium thiosulphate, sodium nitrite, amyl nitrite) have been reported. Hydroxocobalamin and sodium thiosulfate differ from alternatives in having few adverse effects, and on the basis of current evidence are the antidotes of choice.5,12
Recommendations
Patients with severe cardiotoxicity (cardiac arrest, cardiovascular instability, metabolic acidosis, or altered mental status) caused by known or suspected cyanide poisoning should receive cyanide antidote therapy in addition to standard resuscitation guidelines (Good Practice Statement).
ANZCOR recommends that adult patients with suspected severe cyanide poisoning (including those in cardiac arrest) should receive immediate parenteral hydroxocobalamin and sodium thiosulphate (expert advice on dosing required) (Good Practice Statement).
Lipid emulsion for local anaesthetic toxicity
Local anaesthetic toxicity occurs typically in the setting of regional anaesthesia, when a bolus of local anaesthetic inadvertently enters an artery or vein. Systemic toxicity involves the central nervous system, and the cardiovascular system. Severe agitation, loss of consciousness, seizures, bradycardia, conduction blocks, asystole and ventricular tachyarrhythmia can occur. Toxicity can be potentiated in pregnancy, extremes of age, or hypoxaemia.
In addition to standard resuscitation, patients with cardiovascular collapse and cardiac arrest attributable to local anaesthetic toxicity may benefit from treatment with intravenous 20% lipid emulsion.5,13
Recommendations
ANZCOR suggests in addition to standard resuscitation, patients with cardiovascular collapse and cardiac arrest attributable to local anaesthetic toxicity receive 20% lipid emulsion. Give an initial intravenous bolus of 1.5 mL/kg of 20% lipid emulsion followed by an infusion at
15 mL/kg/hr. Give up to three bolus doses of lipid at 5-minute intervals and continue the infusion until the patient is stable or has received up to a total of 12 mL/kg [Good Practice Statement].
Sodium bicarbonate for tricyclic depressant toxicity
Self-poisoning with tricyclic antidepressants and related drugs (e.g. amitriptyline, desipramine, imipramine, nortriptyline, doxepin, and clomipramine) is not as common today as it used to be, but when it occurs it may be associated with hypotension, seizures, coma and life-threatening arrhythmias. Cardiac toxicity is mediated by anticholinergic and sodium channel-blocking effects and can produce a broad-complex tachycardia (VT). Consider tricyclic overdose as a possible diagnosis in adults presenting with an otherwise unexplained shockable rhythm. Hypotension is exacerbated by alpha-1 receptor blockade. Anticholinergic effects include dilated pupils, fever, dry skin, delirium, tachycardia, ileus, and urinary retention. Most life-threatening problems occur within the first 6 hours after ingestion. A widening QRS complex and right axis deviation indicates a greater risk of arrhythmias and can be reversed by serum alkalinisation.
Recommendations
ANZCOR suggests sodium bicarbonate 8.4% 1 to 2 mL/kg up to 100 mL IV, every 3 to 5 minutes, titrated to a narrowing of the QRS complex (aim for serum pH 7.45 to 7.55). Maximum total dose is 6 mL/kg (6 mmol/kg) (expert advice on dosing required) (Good Practice Statement).
Alternatively, or in addition hyperventilate an intubated patient aiming for a serum pH between 7.45 and 7.55 (maintaining PaCO2 between 30 and 35 mmHg) (Good Practice Statement).
Abbreviations
|
Abbreviation |
Meaning/Phrase |
|
ABCDE |
Airway, Breathing, Circulation, Disability, Exposure |
|
ALS |
advanced life support |
|
ARC |
Australian Resuscitation Council |
|
ASCIA |
Australasian Society of Clinical immunology and Allergy |
|
ANZCA |
Australian and New Zealand College of Anaesthetists |
|
ANZCOR |
Australian and New Zealand Committee on Resuscitation |
|
ANZSCTS |
Australasian Australian and New Zealand Society of Cardiac and Thoracic Surgeons |
|
ANZICS |
Australian and New Zealand Intensive Care Society |
|
ANZAAG |
Australian and New Zealand Anaesthetic Allergy Group |
|
BLS |
basic life support |
|
CALS |
cardiothoracic advanced life support |
|
CoSTR |
Consensus on Science with Treatment Recommendations |
|
CPR |
cardiopulmonary resuscitation |
|
ECLS |
extracorporeal life support |
|
ECMO |
extracorporeal membrane oxygenation |
|
ECPR |
extracorporeal cardiopulmonary resuscitation |
|
EtCO2 |
end-tidal CO2 |
|
ICU |
Intensive care unit |
|
IHCA |
in-hospital cardiac arrests |
|
IM |
intramuscular |
|
IN |
intranasal |
|
IO |
intraosseous |
|
IV |
intravenous |
|
OHCA |
out-of-hospital cardiac arrests |
|
PCI |
percutaneous coronary intervention |
|
PE |
pulmonary embolism |
|
PEEP |
positive end-expiratory pressure |
|
PPE |
personal protective equipment |
|
NZRC |
New Zealand Resuscitation Council |
|
RCT |
randomised control trial |
|
ROSC |
return of spontaneous circulation |
|
SC |
subcutaneous |
|
VF |
ventricular fibrillation |
|
VT |
ventricular tachycardia |
References
- Cardona V, Ansotegui I, Ebisawa M, et al, on behalf of the World Allergy Organisation Anaphylaxis Committee. Anaphylaxis Guidance 2020. World Allergy Organization Journal 2020; doi:10.1016/j.waojou.2020.100472
- https://www.allergy.org.au/hp/papers/acute-management-of-anaphylaxis-guidelines
- https://www.anzca.edu.au/safety-advocacy/standards-of-practice/perioperative-anaphylaxis-management-guidel
- https://www.resus.org.uk/library/additional-guidance/guidance-anaphylaxis
- Deakin CD, Morrison LJ, Morley PT, Callaway CW, Kerber RE, Kronick SL, Lavonas EJ, Link MS, Neumar RW, Otto CW, Parr M, Shuster M, Sunde K, Peberdy MA, Tang W, Hoek TLV, Böttiger BW, Drajer S, Lim SH, Nolan JP. Part 8: Advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. [doi: DOI: 10.1016/j.resuscitation.2010.08.027]. 2010;81(1, Supplement 1):e93-e174.
- Boyd J, Brugger H, Shuster M. Prognostic factors in avalanche resuscitation: a systematic review. Resuscitation. 2010 Jun;81(6):645-52.
- Karcher C, Jurisevic C, Southwood T, et al. The Australasian ANZSCTS/ANZICS guidelines on cardiothoracic advanced life support (CALS-ANZ). Crit Care Resusc 2022; doi: 10.51893/2022.3.SA3.]
- Soar J, Callaway C, Aibiki M, Böttiger BW, Brooks SC, Deakin CD, Donnino MW, Drajer S, Kloeck W, Morley PT, Morrison LJ, Neumar RW, Nicholson TC, Nolan JP, Okada K, O’Neil BJ, Paiva EF, Parr MJ, Wang TL, Witt J, on behalf of the Advanced Life Support Chapter Collaborators. Part 4: Advanced life support. 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2015;95:e71–e1203
- Soar J, Berg KM, Andersen LW et al. 4: Adult Advanced Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2020;156:A80-A119. https://doi.org/10.1016/j.resuscitation.2020.09.012
- Greif R, Bray JE, Djärv T et al. 2024 International Consensus on Cardiopulmonary Resuscitation and Emergency 2 Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2024;205:110414.
- Jeejeebhoy FM, Zelop CM, Windrim R, Carvalho JC, Dorian P, Morrison LJ. Management of cardiac arrest in pregnancy: A systematic review. Resuscitation. 2011 Jul;82(7):801-9.
- Reade MC, Davies S, Morley PT, Dennett J, Jacobs I. Management of cyanide poisoning: a systematic review. (submitted for publication 2011). EMA, 2012,24:225-238
DOI: 1111/j.1742-6723.2012.01538.xPMID: 22672162 - S-H, J-M, Lee SH and Sohn J-T. Lipid Emulsion for Treating Local Anaesthetic Systemic Toxicity. Int J Med Sci. 2018; 15(7): 713–722.
About this Guideline
|
Search date/s |
See ILCOR PICOs in CoSTR documents http://ilcor.org |
|
Questions/PICOs: |
See ILCOR PICOs in CoSTR documents http://ilcor.org |
|
Method: |
GRADE for ILCOR CoSTR reviews. |
|
Main changes: |
Anaphylaxis update to include initial and refractory management algorithms. Endorsement of Australasian Australian and New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) and Australian and New Zealand Intensive Care Society (ANZICS) guidelines on cardiothoracic advanced life support (CALS-ANZ). Hypothermia section included. Tension pneumothorax included. Trauma now covered by Guideline 11.10.1 Management of cardiac arrest due to trauma. |
|
Primary reviewers: |
Michael Parr; Margaret Nicholson, Tonia Nicholson, Sharon-Ann Shunker |
|
Other consultation: |
ASCIA for anaphylaxis. |
|
Worksheet: |
N/A |
|
Approved: |
April 2025 |
|
Guideline Superseded: |
November 2011 |
Referencing this guideline
When citing the ANZCOR Guidelines we recommend:
ANZCOR, 2026, Guideline 11.10 Resuscitation in special circumstances, accessed 7 March 2026, https://www.anzcor.org/home/adult-advanced-life-support/guideline-11-10-resuscitation-in-special-circumstances


