Search
Guideline 11.10.1 Management of Cardiac Arrest due to Trauma
Summary

To whom does this guideline apply?
This guideline applies to adult and paediatric patients in cardiac arrest, or peri-arrest, due to physical trauma. Specific isolated traumatic mechanisms such as near-hanging and burns are not addressed.
Who is the audience for this guideline?
This guideline applies to first-aiders, prehospital clinicians and hospital teams.
Recommendations
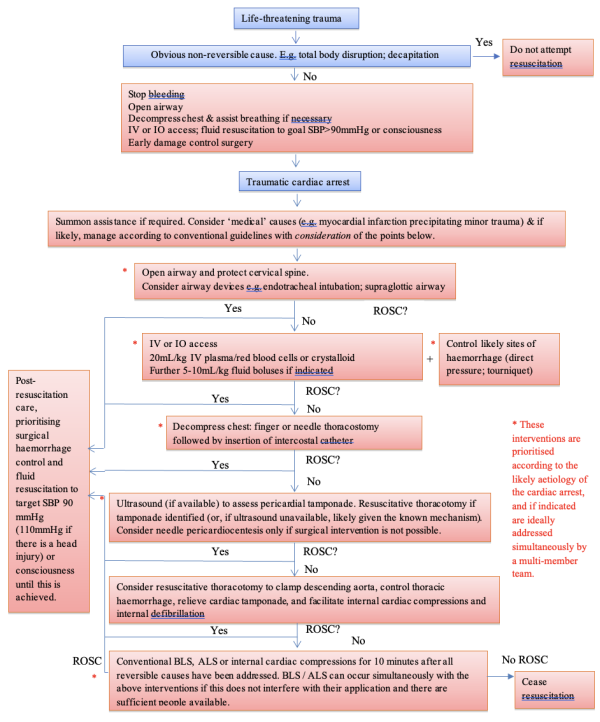
The Australian and New Zealand Committee on Resuscitation (ANZCOR) recommends:
- Unless there are injuries obviously incompatible with life, attempted resuscitation of patients with cardiac arrest due to trauma is not futile and should be attempted.
- The first priority in peri-arrest trauma patients is to stop any obvious bleeding.
- Depending on the likely aetiology of the cardiac arrest, restoration of the circulating blood volume may have a higher priority than airway and breathing. If hypovolaemia is likely, an initial fluid bolus of 20mL/kg should be given as rapidly as possible.
- All patients in cardiac arrest with suspected chest trauma who are not responding to airway opening and restoration of circulating blood volume should have their chest decompressed.
- Surgical drainage of traumatic cardiac tamponade (with repair of cardiac laceration if required) is preferable to needle pericardiocentesis.
- Cardiac arrest due to penetrating trauma is more likely to respond to emergency thoracotomy than is true in blunt trauma. A favourable outcome is rarely possible (even in penetrating trauma) if thoracotomy is initiated more than 10 minutes after the onset of cardiac arrest.
- Cardiac arrest due to isolated head injury, crush syndrome and commotio cordis are special circumstances necessitating specific therapies.
- In cardiac arrest due to trauma, haemorrhage control, restoration of circulating blood volume, opening the airway and relieving tension pneumothorax should have priority over conventional cardiopulmonary resuscitation (CPR) (i.e. external chest compressions, defibrillation and adrenaline) unless a medical cause for cardiac arrest is reasonably suspected to have preceded the traumatic event. However, if there are sufficient resources available and this does not interfere with necessary procedures, conventional CPR should occur simultaneously.
- Prolonged (>10 minutes) CPR in traumatic cardiac arrest after reversible causes have been addressed is almost never associated with a good outcome.
Most deaths due to trauma occur in the first five minutes following the traumatic event, and most of these deaths cannot be prevented, even with skilled and timely treatment.
There are, however, three common causes of preventable early death in trauma:
- Airway obstruction
- Tension pneumothorax
- Haemorrhage
Post-mortem studies of military trauma suggest haemorrhage is responsible for around 60% of preventable deaths amongst patients who actually died following trauma, with 33% due to tension pneumothorax and 7% due to airway obstruction.1 Civilian data is similar, but also identifies cardiac tamponade as the cause of traumatic cardiac arrest in 10% of patients.2 These figures are often quoted with the suggestion that they should determine priorities for intervention in trauma, but this is misleading. Based on post-mortem studies, these figures do not account for patients who would have died were it not for successful interventions such as airway control. Opening the airway (in particular) is likely to be proportionately more important than these figures suggest.
While patients in cardiac arrest due to trauma have a worse prognosis than other cardiac arrest patients, several large series show survival after appropriate treatment is possible, with recent studies showing 5.1%3, 6.6%4, 7%5 and 7.5%6 survival to discharge, albeit with varying rates of neurological recovery (2%5 to 6.6%4). Therefore, unless there are injuries or wounds that are obviously incompatible with life (such as substantial body disruption), attempted resuscitation of patients with cardiac arrest due to trauma is not futile and should be attempted (Class A, LOE III). Conversely, prolonged (>10 minutes) cardiopulmonary resuscitation after reversible causes have been addressed is almost never associated with a good outcome.
This guideline applies to first-aiders, prehospital clinicians and hospital teams managing trauma patients who are peri-arrest or in cardiac arrest. However, the equipment, skills and experience required to provide many of the interventions described will not exist in all circumstances. Nothing in this guideline suggests that first-aiders or clinicians should work outside their scope of practice, or perform procedures for which they have insufficient training. Particularly with respect to highly invasive procedures such as resuscitative thoracotomy, the risk to a patient from a procedure performed incorrectly or for a presumed indication that is, in reality, not present may be greater than not attempting such a procedure. No fault should be attributed to clinicians who, by remaining within their scope of practice, do not perform one of the procedures this guideline recommends or lists for consideration.
Pre-Arrest: Stop the Bleeding

Trauma patients who are able to maintain their circulation may have injuries or wounds that will lead to cardiac arrest if not adequately treated. The first priority in such patients is to stop the bleeding using one of the techniques in ANZCOR Guideline 9.1.1 or (in hospital) more advanced interventions such as surgical exploration or interventional radiology. Only after such interventions are commenced should attention be directed to the airway or breathing (Class A, LOE IV), unless there are sufficient people to perform interventions simultaneously.
Airway

ANZCOR Guideline 11.6 describes basic and advanced techniques to open the airway. A further consideration in trauma is the possibility of cervical spine injury, the assessment and management of which is described in ANZCOR guideline 9.1.6.
A patient in cardiac arrest due to trauma should have the airway opened as quickly as possible while not delaying blood volume expansion and relief of possible tension pneumothorax. Chin lift / jaw thrust are preferred techniques but head tilt and / or positioning in the recovery position (likely to be associated with more cervical spine movement) may be required. (Class B, LOE IV).
Direct trauma to the airway may contraindicate usual supraglottic approaches. Therefore, insertion of an endotracheal, tracheostomy or purpose-designed cricothyroidotomy tube through the cricothyroid membrane or trachea may be required. Whether these procedures should take priority over restoration of the circulating blood volume will depend on the likely principal cause of the cardiac arrest or impending arrest.
Restoration of Circulating Blood Volume

Depending on the condition of the patient and the likely aetiology of the cardiac arrest, restoration of the circulating blood volume may be the highest priority for patients in cardiac arrest due to trauma.
Intravenous or intraosseous access

Intravenous or intraosseous access should be established as rapidly as possible. If peripheral intravenous cannulation can be accomplished prior to cardiac arrest, ideally two cannulae of at least 18G should be inserted (Class A, LOE IV).
Peripheral venous cannulation is likely to be impossible in cardiac arrest due to exsanguination, regardless of whether or not cardiac compressions are being performed. In adults, central venous cannulation may be possible and should be attempted using a Seldinger technique and a short, large-bore catheter (such as a catheter-introducer for a pulmonary artery catheter or a dialysis catheter) (Class B, LOE IV). Small-bore central venous catheters are not recommended due to their low maximal flow rates. One study found subclavian central venous cannulation more likely to be successful (success in 94% of attempts) than femoral venous cannulation (success in only 77%)7. In young children, intraosseous (IO) access is preferred to central venous access.
IO access may be more rapidly and reliably achieved than venous access, especially by clinicians inexperienced with central venous catheter insertion, and especially in children. In adults, IO cannulae in the sternum or humeral head achieve more rapid fluid administration than those in the medial proximal tibia.8 In children, IO cannulae should be placed in either the humeral head or medial proximal tibia. Two IO access devices may be warranted to increase the maximum possible rate of fluid infusion. The choice between central IV, peripheral IV and IO access will depend on the condition of the patient and the equipment and personnel available; there is no evidence-based threshold time at which attempted IV access should be abandoned in favour if IO access. When sufficient clinicians are available, simultaneous approaches are suggested.
Fluid therapy

If hypovolaemia is a possible cause or contributor to traumatic cardiac arrest, an initial (ideally warmed) fluid bolus of 20mL/kg (approximately 1.4L in a 70kg patient) should be given as rapidly as possible (Class B; LOE IV). In exsanguinating haemorrhage, this should be a 1:1 or 1:2 mixture of thawed (Class B; LOE III) thawed fresh-frozen plasma : packed red blood cells.9,10 Use of other blood products (such as cryoprecipitate and platelets) should be guided by an institutional Massive Transfusion Protocol informed by consensus guidelines,9 and in particular should avoid dilution of platelets and fibrinogen. Several ambulance services have shown that prehospital administration of packed red blood cells and plasma is feasible. Administration of large volumes of packed red blood cells anticoagulated with citrate will reduce plasma ionised calcium, necessitating replacement with calcium gluconate or calcium chloride, ideally titrated to measured levels.
If blood products are not available, a crystalloid solution should be used. Blood products should be substituted for crystalloid as soon as possible.
Further fluid boluses of 5-10mL/kg should be given if hypovolaemia is suspected as the ongoing cause of persistent cardiac arrest. (Class B; LOE IV).
In adults, once spontaneous cardiac output is restored, prior to surgical haemorrhage control and at least for the first hour, further fluid should be titrated either to a systolic blood pressure of 90mmHg (permissive hypotension) or to consciousness. (Class B; LOE IV). Due to the risk of raised intracranial pressure reducing cerebral perfusion pressure, a patient with substantial trauma to the head may benefit from a target systolic blood pressure of 110mmHg. (Class B; LOE IV). The optimal endpoint of fluid resuscitation after the first hour or after surgical haemorrhage control is unclear; however, progressive improvements in plasma lactate and base deficit are reasonable targets in the absence of advanced haemodynamic monitoring. Achieving such targets may require a higher target systolic blood pressure than during the first hour hypotensive resuscitation phase. Acidosis should not be corrected with IV sodium bicarbonate (Class B; LOE IV) unless it is used as a specific treatment for hyperkalaemia, as (for example) in crush syndrome. In children, there is insufficient evidence for or against a strategy of permissive hypotension during the first hour of resuscitation. Resuscitation targeting a low to normal (for age) systolic pressure for age is recommended in the absence of such evidence.
Haemorrhage control

A patient in traumatic cardiac arrest will have little active bleeding. However, bleeding may resume upon restoration of circulation. Therefore, during the resuscitation phase but without delaying the other effective interventions listed here, the haemorrhage control techniques listed in ANZCOR Guideline 9.1.1, such as direct wound pressure, proximal arterial tourniquets, pelvic binders, junctional haemorrhage devices and haemostatic dressings, should be applied.
Chest Decompression

All patients in cardiac arrest with suspected chest trauma who are not responding to airway opening and restoration of circulating blood volume should have their chest decompressed as described below. (Class B; LOE IV). Resuscitative thoracotomy may be indicated in limited situations.
Finger thoracostomy (initially on the most affected side of the chest) is the preferred method of chest decompression. Finger thoracostomy involves incising 3-4cm of skin over the 4th intercostal space just anterior to the mid-axillary line followed by blunt dissection to the pleura to allow introduction of a finger into the pleural space. This should be followed by insertion of an intercostal catheter if available. Intercostal catheters should be connected to underwater seal drains or one-way valves. If an intercostal catheter is not available, an adhesive one-way chest seal is acceptable. The same procedure should be performed on the contralateral side if there is suspicion of bilateral tension pneumothoraces. If more than 1000mL blood drains immediately, or there is ongoing bleeding >200mL/hr for the subsequent 2-4 hours, surgical exploration is warranted. (Class B; LOE IV). Finger thoracostomies should be accompanied by intubation and mechanical ventilation because of the risk of inadequate ventilation due to air entering the pleural space. (Class B; LOE IV).
An alternative to finger thoracostomy that may allow more rapid chest decompression in some circumstances is insertion of a long, large bore (ideally 8cm, 12- or 14-gauge) cannula into the pleural cavity. The optimal location for cannula insertion is unknown, and probably depends on individual body habitus.
Options include the second intercostal space at or just lateral to the midclavicular line, with the needle directed away from the heart, or alternatively the 4th or 5th intercostal space just anterior to the mid-axillary line. (Class B; LOE IV). If resuscitation continues, needle chest decompression must always be followed by insertion of an intercostal catheter.
Pericardiocentesis

The commonest cause of pericardial tamponade due to trauma is a penetrating injury or wound to the myocardium, which will require surgical intervention via thoracotomy. Urgent bedside echocardiography should be used to identify or exclude pericardial tamponade due to trauma (Class B; LOE IV).
Needle pericardiocentesis is almost never the optimal means of decompressing the pericardium in trauma, as it does not address the commonest cause (myocardial laceration) and because pericardial blood is often clotted, preventing aspiration. However, when no surgeon or other clinician with the required skills and experience is present to surgically manage the patient, needle pericardiocentesis (ideally under ultrasound guidance) can be attempted in a patient who is peri-arrest or in cardiac arrest with a high suspicion of cardiac tamponande (Class B; LOE IV).
Resuscitative Thoracotomy

A resuscitative thoracotomy can:
- release tension pneumothorax or cardiac tamponade;
- allow direct control of intrathoracic haemorrhage;
- allow cross-clamping the descending aorta (in so doing stopping blood loss below the diaphragm and improving brain and cardiac perfusion); and
- permit open cardiac compression and defibrillation.
In one case series, resuscitative thoracotomy was successfully performed by adequately trained and experienced prehospital clinicians.6 However, in general in the Australian and New Zealand civilian context this will remain a hospital intervention performed by a surgeon or a specifically trained and experienced emergency or critical care physician. Whether a clam-shell or anterolateral approach is best will be determined by the pattern of injury or wounding and the available surgical expertise. The decision on proceeding with resuscitative thoracotomy will rest on the mechanism of injury or wounding, whether there is likely to be a surgically-correctable problem given the expertise and resources available, and the duration since the traumatic event and the onset of cardiac arrest. Ideally, hospitals should develop local guidelines relevant to their institution.
As a general guide, cardiac arrest due to penetrating trauma is more likely to respond to emergency thoracotomy than cardiac arrest due to blunt trauma. A favourable outcome is rarely possible (even in penetrating trauma) if resuscitative thoracotomy is initiated more than 10 minutes after the onset of cardiac arrest. (Class A; LOE IV).
A resuscitative thoracotomy may be indicated prior to cardiac arrest – if time allows, ideally by an appropriately trained surgical team in an adequately-equipped operating theatre.
Special Circumstances

Crush syndrome

ANZCOR Guideline 9.1.7 outlines the recommended early management of a patient with crush injury. In addition to the Basic Life Support (BLS) measures outlined in that guideline, Advanced Life Support (ALS) for a crushed patient in cardiac arrest or peri-arrest should consider the possibility of hyperkalaemia as a contributing aetiology. ANZCOR recommends urgent check of the serum potassium level if possible, with urgent treatment indicated for potassium levels >6.5 mmol/L. ECG changes (peaked T waves, loss of P waves, prolonged QRS interval, or a “sine wave” appearance) prior to cardiac arrest also suggest hyperkalaemia. In the absence of diagnostic tests, empiric treatment on the basis of trauma mechanism alone may be required. Treat a crushed patient with cardiac arrest due to hyperkalaemia with:
- Calcium chloride 10% 5-10mL or calcium gluconate 10% 10-20mL IV. (weight adjust for children);
- Glucose 50% 50mL and (simultaneously) insulin 10 units IV (weight adjust for children); and/or
- Sodium bicarbonate 1mmol/kg IV.
(Class A; LOE IV).
Direct cardiac trauma resulting in commotio cordis

Commotio cordis occurs when a force applied to the anterior chest precipitates cardiac arrhythmia, most commonly ventricular fibrillation. The most common precipitant is being struck by a hard ball during sport. Cardiac arrest due to commotio cordis is greatest when a force is applied at 65 kilometres per hour,11 with the chance of structural heart damage increasing at greater velocities. Suspected traumatic cardiac arrest due to commotio cordis should be managed according to the general principles for CPR outlined in ANZCOR Guideline 11.2, with early defibrillation of shockable rhythms accorded the same high priority (Class A; LOE IV).
Isolated major head injury

Isolated traumatic brain injury (TBI) without substantial structural brain pathology has been noted in case series and animal models occasionally to cause apnoea associated with a transient catecholamine surge followed by cardiovascular collapse.12 Several unconscious apnoeic TBI patients with preserved spontaneous circulation have reportedly been resuscitated, with complete neurological recovery, by means of artificial respiration alone. Whether spontaneous respiration might have resumed prior to hypoxic cardiac arrest in these patients remains speculative. However, artificial respiration of an apnoeic patient requires little justification. In the absence of other injuries, such patients should be managed according to the general principles for CPR outlined in ANZCOR Guideline 11.2.
Conventional Basic and Advanced Life Support

A small minority of patients will have a medical cause that precipitates cardiac arrest that is followed by trauma: for example, in drivers involved in road traffic accidents. If the severity of the trauma mechanism or injuries observed appear insufficient to have caused cardiac arrest, a medical cause (such as myocardial infarction) should be suspected and managed according to the general principles for CPR outlined in ANZCOR Guidelines 6 and 11.2.
In cardiac arrest due to trauma, all of the interventions aimed at addressing underlying causes take priority over chest compressions, defibrillation and adrenaline. However, if there are sufficient resources available and there is no interference with essential procedures, conventional CPR can occur simultaneously. The effectiveness of conventional CPR will depend on correcting the causes of the cardiac arrest.
External Chest Compressions

An exsanguinated patient theoretically derives little benefit from external cardiac compressions until blood volume is restored to a minimally sufficient quantity. External chest compressions may exacerbate haemorrhage and cardiac tamponade, and positive pressure ventilation may further reduce critically low venous return or cause air embolism.13 Several case series demonstrate that external chest compressions are virtually never effective for patients in traumatic cardiac arrest unless the underlying cause of the arrest is simultaneously and rapidly addressed.13-16 Conversely, there is no clinical evidence that chest compressions worsen outcome in trauma. Therefore, external chest compressions (as recommended in ANZCOR Guideline 6) should be commenced as a secondary priority, after airway opening, commencement of restoration of circulating blood volume (if the required equipment is available), and (if appropriate) decompression of the chest (Class B; LOE IV). If there is any other indication for resuscitative thoracotomy and this is possible in the circumstances, internal cardiac compression is preferable to external chest compressions.17 (Class A; LOE IV).
In the absence of the requisite equipment or expertise to address the underlying aetiology of cardiac arrest in trauma, first aiders should summon skilled assistance then proceed directly to BLS.
Adrenaline

There is little evidence for or against the use of adrenaline in cardiac arrest due to trauma. Retrospective observational studies have found vasopressor use associated with worse outcome in haemorrhagic shock,18,19 but conversely, a large case series found patients in established traumatic cardiac arrest had a higher chance of survival to hospital discharge if they were treated with adrenaline.20 Such studies are almost certainly confounded by residual indication bias despite attempts at adjustment for severity of injury, and there have been no prospective clinical trials. Guidance is therefore based on extrapolation from physiological principles.
ANZCOR does not recommend adrenaline for patients in traumatic cardiac arrest until haemorrhage control, opening the airway, commencement of restoration of circulating blood volume and (if appropriate) decompression of tension pneumothorax have been addressed. (Class A; LOE IV).
Once spontaneous cardiac output is restored, hypotension is usually the result of hypovolaemia and should be treated initially with ongoing volume replacement. (Class B; LOE IV). In the later phases of post-arrest care, vasodilation or myocardial depression may require adrenaline or other vasoactive infusions.
Defibrillation

Only 7.5% of patients in traumatic cardiac arrest are initially found in VF or VT.21 Therefore defibrillation is not the priority for the majority of trauma patients in cardiac arrest. ANZCOR suggests not using defibrillation prior to opening the airway, commencement of restoration of circulating blood volume, and (if appropriate) decompression of the chest (Class B; LOE IV). In the small minority of patients who are in traumatic cardiac arrest with VF or VT, reversible causes must be addressed, and defibrillation should be performed promptly, especially in those suspected of having a cardiac co-morbidity. (Class A; LOE IV).
Four Hs and Four Ts

ANZCOR Guideline 11.2 recommends consideration of “Four Hs and four Ts” (hypoxaemia, hypovolaemia, hyper/hypokalaemia and other metabolic disorders, hypo/hyperthermia, tension pneumothorax, tamponade, toxins, and thrombosis – pulmonary / coronary) in any patient in cardiac arrest, particularly those in asystole. Following this cardiac arrest due to trauma guideline will identify and treat all these conditions, with the exceptions of hypo/hyperthermia, toxins and thrombosis. These relatively infrequent causes should be considered in a patient who has not responded to other interventions. (Class A, LOE IV).
Transport to Hospital

Several potentially effective interventions (such as resuscitative thoracotomy) may only be available in hospital, suggesting speed of transport should be prioritised over time taken performing prehospital interventions. Conversely, the case series demonstrating the highest survival rates after traumatic cardiac arrest reported on protocols that mandated not leaving the incident scene until spontaneous circulation was restored.4 On the basis of the best available evidence, ANZCOR suggests that patients in cardiac arrest due to trauma should only be transported to hospital after return of spontaneous circulation, unless the hospital is in such close proximity that a patient thought to require an emergency room thoracotomy would have a realistic chance of this occurring within 10 minutes.
Patients who have a cardiac arrest due to trauma during transportation should have the interventions described in this guideline, noting that those who have no spontaneous circulation for >10 minutes are unlikely to survive.
In the current Australian and New Zealand civilian context, a prehospital resuscitative thoracotomy will rarely, if ever, be appropriate. (Class B; LOE IV).
Terminating Attempted Resuscitation

There is no consensus on how long resuscitation attempts should continue after cardiac arrest due to trauma. Most case series of traumatic cardiac arrests do not report informative time data. Restoration of a circulating blood volume sufficient to sustain spontaneous circulation may take several minutes, depending on the equipment and venous access available. In the absence of data, ANZCOR recommends continuation of BLS or ALS (including external cardiac compressions) for up to 10 minutes after these potentially reversible causes have been addressed, following which resuscitation attempts should be stopped if there is no ROSC. (Class A; LOE IV).
Debriefing

The circumstances of the traumatic event and the physical appearance of the patient can be more distressing to first aiders and clinicians than might be the case for victims of cardiac arrest due to non-traumatic causes. Sensitive, professional debriefing of people involved in resuscitation efforts is likely to have value.
Advice to First-Aiders

Many of the potentially beneficial interventions for patients in cardiac arrest due to trauma will only be possible for trained prehospital clinicians or hospital personnel with the required equipment. Speed of ambulance arrival to a patient in traumatic cardiac arrest is a strong predictor of survival. Therefore, first-aiders and clinicians lacking necessary equipment should prioritise calling for skilled help over attempting BLS (Class A; LOE IV). Conversely, first-aiders can apply simple interventions that might effectively prevent the progression to cardiac arrest after trauma – in particular, opening the airway (ANZCOR Guideline 4) and stopping the bleeding (ANZCOR Guideline 9.1.1) (Class A; LOE IV).
Further reading

ANZCOR Guideline 9.1.1 Principles for the Control of Bleeding for First Aiders
ANZCOR guideline 9.1.6 Management of Suspected Spinal Injury
ANZCOR Guideline 9.1.7 Emergency Management of a Crushed Victim
ANZCOR Guideline 11.2 Protocols for Adult Advanced Life Support
ANZCOR Guideline 11.6 Equipment and Techniques in Adult Advanced Life Support
Summary

References

- Champion HR, Bellamy RF, Roberts CP, Leppaniemi A. A profile of combat injury. J Trauma 2003;54:S13-S9.
- Kleber C, Giesecke MT, Lindner T, Haas NP, Buschmann CT. Requirement for a structured algorithm in cardiac arrest following major trauma: epidemiology, management errors, and preventability of traumatic deaths in Berlin. Resuscitation 2014;85:405-10.
- Deasy C, Bray J, Smith K, et al. Traumatic out-of-hospital cardiac arrests in Melbourne, Australia. Resuscitation 2012;83:465-70.
- Leis CC, Hernandez CC, Blanco MJ, Paterna PC, Hernandez RE, Torres EC. Traumatic cardiac arrest: should advanced life support be initiated? J Trauma Acute Care Surg 2013;74:634-8.
- Grasner JT, Wnent J, Seewald S, et al. Cardiopulmonary resuscitation traumatic cardiac arrest--there are survivors. An analysis of two national emergency registries. Crit Care 2011;15:R276.
- Lockey D, Crewdson K, Davies G. Traumatic cardiac arrest: who are the survivors? Ann Emerg Med 2006;48:240-4.
- Emerman CL, Bellon EM, Lukens TW, May TE, Effron D. A prospective study of femoral versus subclavian vein catheterization during cardiac arrest. Ann Emerg Med 1990;19:26-30.
- Boswell K, Dubose JJ, Matsura M. Intraosseous infusion rates under high pressure: a cadaver study of anatomical site comparisons. Advanced Technology Applications in Combat Casualty Care; 2012.
- Patient blood management guidelines module 1: critical bleeding / massive transfusion. Canberra: National Health and Medical Research Council; 2011.
- Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 2015;313:471-82.
- Link MS, Maron BJ, Wang PJ, Vanderbrink BA, Zhu W, Estes NA, III. Upper and lower limits of vulnerability to sudden arrhythmic death with chest-wall impact (commotio cordis). J Am Coll Cardiol 2003;41:99-104.
- Wilson MH, Hinds J, Grier G, Carley S, Davies G. Impact brain apnoea - a forgotten cause of cardiovascular collapse in trauma. Resuscitation 2016; in press.
- Mattox KL, Feliciano DV. Role of external cardiac compression in truncal trauma. J Trauma 1982;22:934-6.
- Alanezi K, Alanzi F, Faidi S, et al. Survival rates for adult trauma patients who require cardiopulmonary resuscitation. CJEM 2004;6:263-5.
- Battistella FD, Nugent W, Owings JT, Anderson JT. Field triage of the pulseless trauma patient. Arch Surg 1999;134:742-5.
- Rosemurgy AS, Norris PA, Olson SM, Hurst JM, Albrink MH. Prehospital traumatic cardiac arrest: the cost of futility. J Trauma 1993;35:468-73.
- Twomey D, Das M, Subramanian H, Dunning J. Is internal massage superior to external massage for patients suffering a cardiac arrest after cardiac surgery? Interact Cardiovasc Thorac Surg 2008;7:151-6.
- Collier B, Dossett L, Mann M, et al. Vasopressin use is associated with death in acute trauma patients with shock. J Crit Care 2010;25:173-14.
- Plurad DS, Talving P, Lam L, Inaba K, Green D, Demetriades D. Early vasopressor use in critical injury is associated with mortality independent from volume status. J Trauma 2011;71:565-70.
- Chiang WC, Chen SY, Ko PC, et al. Prehospital intravenous epinephrine may boost survival of patients with traumatic cardiac arrest: a retrospective cohort study. Scand J Trauma Resusc Emerg Med 2015;23:102.
- Lin CH, Chiang WC, Ma MH, Wu SY, Tsai MC, Chi CH. Use of automated external defibrillators in patients with traumatic out-of-hospital cardiac arrest. Resuscitation 2013;84:586-91.


